Signs of Infection After Oral Surgery in Diabetic Patients

Oral surgery can be safely performed for diabetic patients, but healing requires closer monitoring due to how diabetes affects circulation, inflammation, and immune response. After procedures involving extractions or surgical removal—especially cases involving wisdom teeth—the risk of infection can be higher if warning signs are missed early.
Understanding what infection looks like after oral surgery allows diabetic patients to act quickly, avoid complications, and support proper healing.
Why Diabetic Patients Face Higher Infection Risk
Diabetes can slow wound healing and reduce the body’s ability to fight bacteria. Elevated blood sugar levels interfere with white blood cell function and can prolong inflammation at the surgical site. When oral surgery involves impacted teeth or multiple extractions—such as when patients are learning how many wisdom teeth they have—the surgical area may take longer to stabilize.
This delay creates an opportunity for bacteria to multiply if post-operative care is not closely followed.
Early Signs of Infection After Oral Surgery
Diabetic patients should observe the surgical area daily, especially within the first week after the procedure.
Pain That Increases Instead of Improves
Mild pain is expected initially, but discomfort should gradually decrease. Pain that worsens after a few days—especially deep or throbbing pain—can signal infection. In some cases, discomfort may radiate toward the throat or jaw, similar to symptoms experienced with throat pain related to wisdom tooth complications.
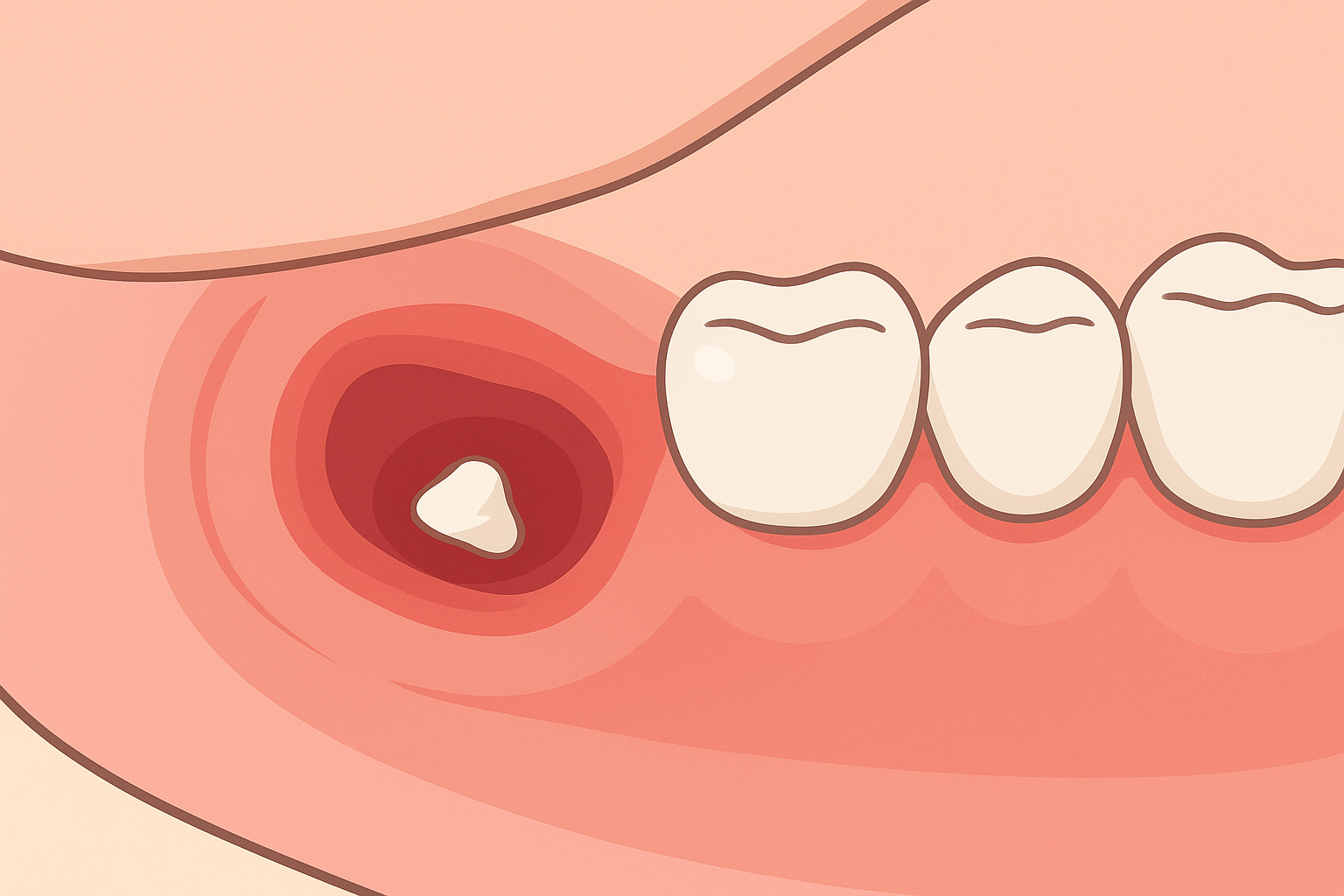
Persistent Swelling
Normal swelling peaks within 48 to 72 hours. Swelling that continues to expand, feels firm, or spreads toward the neck or face may indicate infection rather than normal healing.
Red or Warm Gums
Inflammation that becomes more pronounced, rather than subsiding, is another early warning sign. Diabetic patients may notice redness or warmth around the surgical site that does not resolve.
Advanced Infection Symptoms to Watch Closely
Some infections progress quietly before becoming severe, making awareness especially important for diabetic patients.
Pus or Drainage
Any white, yellow, or foul-smelling discharge from the surgical area is a clear indicator of infection and requires immediate professional evaluation.
Fever or Chills
A low-grade fever may occur after surgery, but ongoing or rising temperature often reflects infection. Diabetes can intensify systemic responses, making fever a critical warning sign.
Delayed Healing
If the surgical site appears open, lacks healthy clot formation, or shows minimal improvement after several days, infection may be interfering with recovery. Poor healing is more common when blood sugar levels fluctuate during recovery.
Other Symptoms Diabetics Should Not Ignore
Persistent Bad Breath
Ongoing bad breath or an unpleasant taste can be caused by bacterial buildup at the surgical site and should not be dismissed as normal post-surgical discomfort.
Blood Sugar Spikes
Infections often cause unexplained increases in glucose readings. Diabetic patients who notice sudden changes should contact both their oral surgeon and primary care provider.
Referred Pain
Infections can cause discomfort beyond the mouth, including ear or jaw pain similar to symptoms associated with ear pain linked to impacted wisdom teeth.
Reducing Infection Risk After Oral Surgery
Preventive care plays a major role in recovery for diabetic patients.
Stable Glucose Control
Maintaining consistent blood sugar levels before and after surgery supports immune function and tissue repair. This is especially important for patients undergoing extractions later in life, such as those experiencing late wisdom tooth eruption.
Anti-Inflammatory Nutrition
Post-operative nutrition affects healing. Incorporating foods known to reduce inflammations before extraction, can support recovery.
Strict Aftercare Compliance
Taking prescribed medications, keeping the area clean, avoiding smoking, and attending follow-up appointments all help reduce infection risk.
When to Contact Your Oral Surgeon Immediately
Diabetic patients should seek immediate care if they experience:
- Increasing pain after initial improvement
- Spreading or hardened swelling
- Fever, pus, or persistent bleeding
- Sudden loss of blood sugar control
Early intervention prevents localized infections from becoming serious complications.
Final Thoughts
Oral surgery recovery for diabetic patients requires awareness, consistency, and prompt response to warning signs. By recognizing infection symptoms early and following post-operative care closely, most diabetic patients heal successfully and maintain long-term oral health.
Close coordination between patient, oral surgeon, and medical provider remains the key to safe outcomes.

Morning vs. Night Oral Care: What Experts Recommend
January 27, 2026
Can Wisdom Teeth Grow Back After Removal?
December 9, 2025

How Oral Health Directly Impacts Your Overall Health
February 12, 2026

Foods That Help Reduce Inflammation Before Extraction
December 3, 2025

Cheap vs Quality Wisdom Tooth Removal: What Really Matters?
December 18, 2025