Can Diabetics Safely Undergo Oral Surgery?

For people living with diabetes, oral health decisions often come with added concern. A common question many patients ask is whether oral surgery is safe and how diabetes may affect healing, infection risk, and overall outcomes. The reassuring answer is yes—diabetics can safely undergo oral surgery when blood sugar levels are well managed and the procedure is carefully planned.
Advances in oral and maxillofacial surgery have made it possible for patients with chronic conditions, including diabetes, to receive safe, predictable treatment. With proper coordination between the patient, oral surgeon, and medical provider, procedures such as extractions, wisdom tooth removal, and dental implants are routinely completed without complications.
This article explains how diabetes affects oral surgery, what precautions are taken, and what diabetic patients can expect before and after treatment.
How Diabetes Affects Oral Health
Diabetes impacts the body’s ability to regulate blood sugar, which in turn influences immune response, circulation, and healing. These factors play a role in oral health and surgical recovery.
People with diabetes may experience increased inflammation, a higher risk of gum disease, and slower healing after dental procedures. Over time, unmanaged oral infections can also make blood sugar control more difficult, creating a cycle that affects overall health.
Is Oral Surgery Safe for Diabetic Patients?
Oral surgery is generally safe for diabetic patients when glucose levels are controlled. The level of risk depends less on the diagnosis itself and more on how well diabetes is managed before and after surgery.
Patients with stable blood sugar levels tend to heal well and experience outcomes similar to those without diabetes. When blood sugar is poorly controlled, the risk of infection and delayed healing increases, which is why oral surgeons place strong emphasis on pre-surgical planning.
Why Diabetics Often Need Oral Surgery
Diabetic patients may need oral surgery for reasons that are common among adults, including severe decay, infections, bone loss, or impacted teeth.
Wisdom Teeth and Diabetes
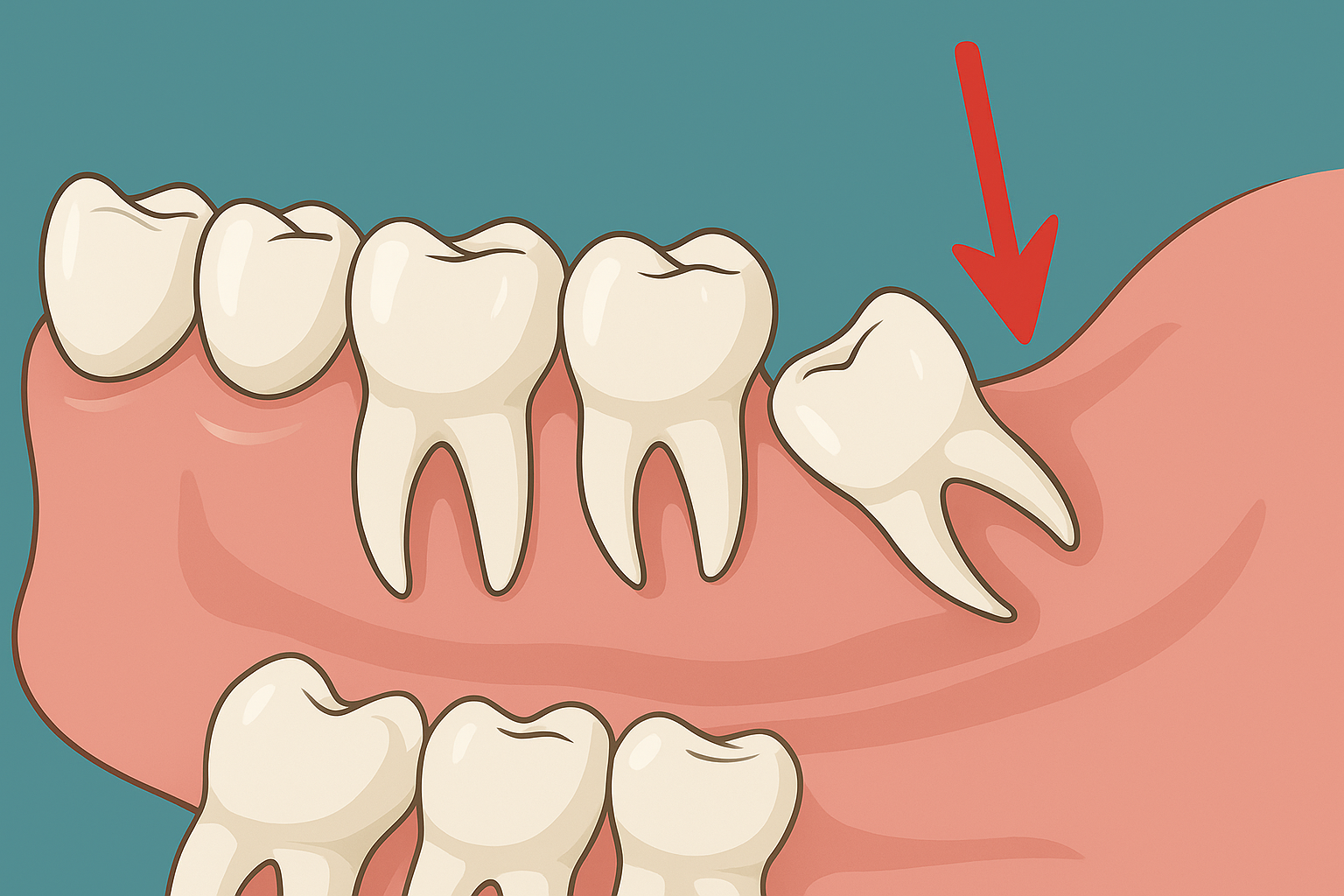
Wisdom teeth are a frequent source of problems when they fail to erupt properly. Knowing the typical wisdom teeth pattern helps explain why crowding and impaction occur and why surgical removal is sometimes necessary.
For diabetic patients, infections around impacted wisdom teeth can escalate more quickly if left untreated, making timely oral surgery an important part of preventing complications.
Preparing for Oral Surgery With Diabetes
Preparation is one of the most important factors in ensuring a safe surgical experience for diabetic patients.
Medical Review and Coordination
Before surgery, the oral surgeon reviews the patient’s medical history, including diabetes type, recent blood glucose readings, HbA1c levels, and medications. In some cases, the surgeon coordinates with the patient’s physician to confirm that blood sugar levels are within a safe range.
Nutrition and Inflammation Control
Diet plays a significant role in healing. Reducing inflammation before surgery supports immune function and recovery, which is why incorporating anti-inflammatory foods before an extraction or surgical procedure can be beneficial for diabetic patients.
Wisdom Tooth Removal for Diabetics
Wisdom tooth surgery is one of the most commonly performed oral procedures and is routinely completed for patients with diabetes.
Infection and Pain Symptoms
When wisdom teeth become impacted or partially erupted, bacteria can collect beneath the gum tissue. This can cause swelling, infection, and even throat pain, which may signal inflammation spreading beyond the immediate surgical site.
Prompt removal reduces the risk of ongoing infection that could interfere with blood sugar control.
Late-Onset Wisdom Tooth Issues
Some adults don’t experience wisdom tooth problems until later in life. Even patients in their 30s or older may develop complications related to late wisdom eruption. Diabetes does not automatically increase surgical risk in these cases, especially when glucose levels are managed.
Referred Pain and Nerve Symptoms
Wisdom tooth inflammation can cause discomfort in areas beyond the jaw. In some cases, ear pain may occur due to shared nerve pathways, making diagnosis and treatment especially important.
Anesthesia and Sedation Considerations
Diabetic patients can safely receive local anesthesia, IV sedation, or general anesthesia depending on the complexity of the procedure and their overall health.
Blood glucose levels are often checked before surgery, particularly when sedation is involved. Medication timing may be adjusted to prevent hypoglycemia or hyperglycemia during the procedure.
Oral surgeons carefully select anesthetic techniques that support patient comfort while maintaining metabolic stability.
Reducing Infection Risk After Surgery
Infection prevention is a key focus when treating diabetic patients.
Modern surgical techniques minimize tissue trauma and promote faster healing. In certain cases, antibiotics may be prescribed to reduce infection risk, and patients are given clear instructions for post-operative care.
Maintaining proper oral hygiene and monitoring blood sugar closely during recovery play an essential role in preventing complications.
Healing and Recovery Expectations
Healing may take slightly longer for some diabetic patients, but most recover without issues when instructions are followed carefully.
Balanced meals, adequate hydration, and consistent glucose monitoring support the healing process. Soft foods that align with diabetes-friendly nutrition plans help maintain stable blood sugar levels while protecting surgical sites.
Patients should contact their oral surgeon if they notice increasing pain, swelling, fever, or delayed healing, as early intervention can prevent more serious problems.
Dental Implants and Diabetes
Dental implants can be a successful long-term solution for diabetic patients with good blood sugar control.
Implant success depends on proper bone healing, known as osseointegration. Stable glucose levels support this process and reduce the risk of implant failure. For many diabetic patients, implants improve chewing efficiency, nutrition, and overall quality of life.
Choosing an Experienced Oral Surgeon
Experience matters when treating patients with diabetes. An oral surgeon familiar with managing medical conditions understands how to adjust surgical planning, anesthesia, and aftercare to reduce risk.
Coordinated care between the surgeon, patient, and medical provider ensures that oral surgery supports overall health rather than compromising it.
Final Thoughts
Diabetes does not prevent patients from safely undergoing oral surgery. With proper preparation, blood sugar control, and expert care, procedures such as wisdom tooth removal and dental implants can be completed successfully.
Addressing oral health issues promptly can reduce chronic inflammation, lower infection risk, and contribute positively to long-term diabetes management.
Can Wisdom Teeth Cause Tooth Misalignment Years Later?
December 15, 2025

How Safe Is Modern Oral Surgery? What Patients Need to Know
December 30, 2025

Your Complete Guide to Choosing the Right Dentist and Treatment
January 22, 2026

Tooth Extraction vs Root Canal: Which Option Works Best for Your Smile?
January 2, 2026

Signs You Might Need a Root Canal
January 15, 2026