What Is an Odontectomy? A Clear Guide to Wisdom Tooth Surgery

If your dentist suggested an odontectomy, you might be wondering exactly what it involves and why it’s necessary. This procedure is a common oral surgery performed to remove impacted or problematic teeth, especially wisdom teeth that haven’t fully erupted or are causing pain. Many patients notice swelling, discomfort, or recurring infections before realizing a surgical solution is needed. Understanding the process and recovery can make the experience much less stressful.
In some cases, persistent discomfort or gum irritation can signal deeper issues. Patients often check guides about tooth infection to understand why a tooth may be causing pain. Similarly, spotting early signs that extraction may be needed helps you prepare mentally and physically for the procedure. Beyond the surgery itself, knowing about long-term options like dental implants, insurance coverage, and treatment costs can help you make informed decisions for lasting oral health.
This guide walks you through the odontectomy procedure step by step, what to expect before and after surgery, and related dental planning so you feel confident and prepared.
What Is an Odontectomy?
An odontectomy is a surgical procedure used to remove a tooth that cannot be easily extracted using standard methods. It is most commonly applied to wisdom teeth, also known as third molars, which often grow at awkward angles or remain partially trapped under the gums.
During an odontectomy, the oral surgeon carefully creates an incision to access the tooth and surrounding bone. Sometimes the tooth is sectioned into smaller pieces to make removal safer and easier. Although the idea of surgery may sound intimidating, this procedure is routine and effective at preventing long-term problems like chronic infection or damage to adjacent teeth.
Why Dentists Recommend an Odontectomy
There are several reasons a dentist or oral surgeon may recommend an odontectomy:
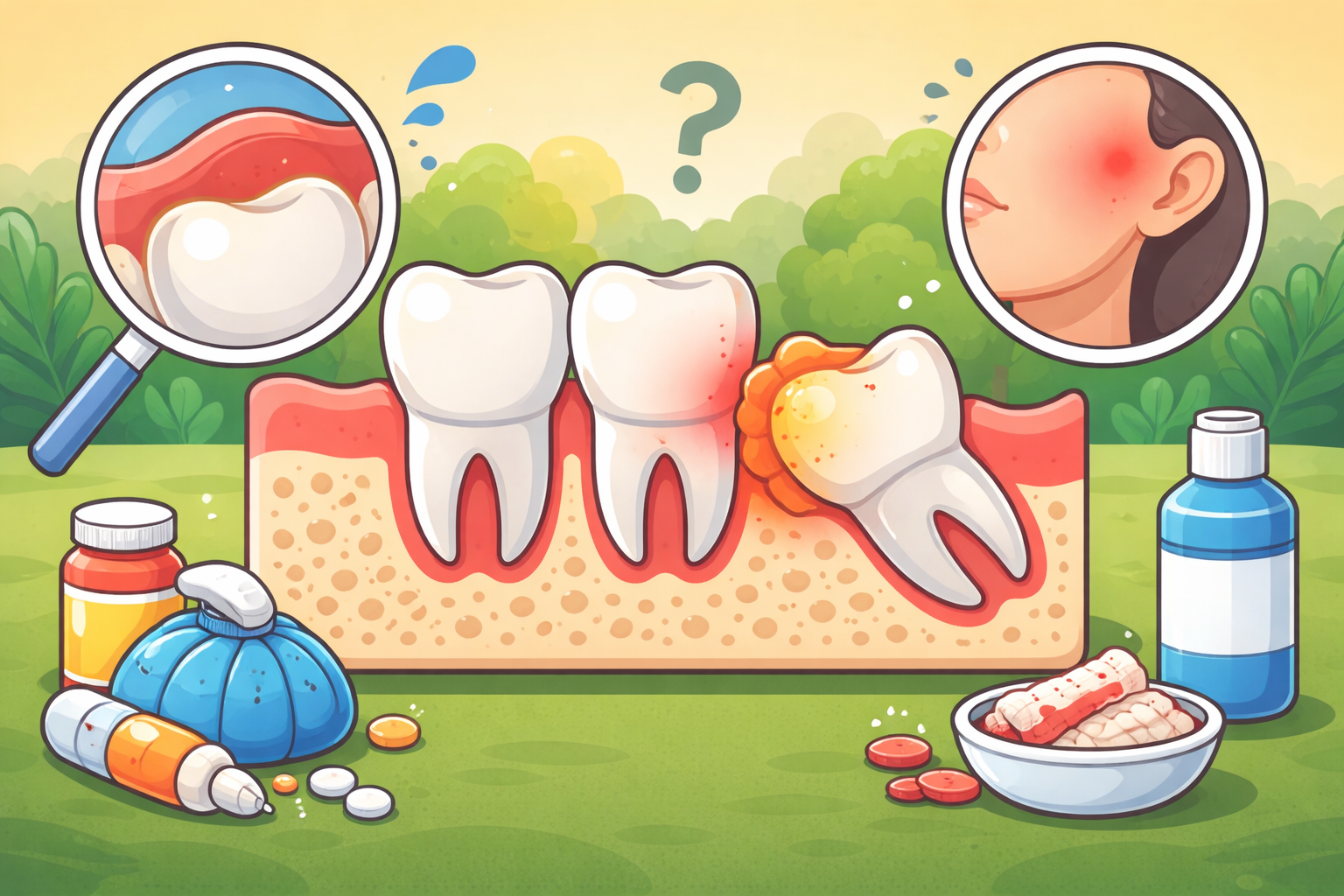
Impacted Wisdom Teeth
Wisdom teeth can become impacted when they don’t have enough room to grow properly. This can lead to pain, swelling, and pressure on nearby teeth. Many patients read guides about tooth infection to determine if impacted teeth are causing recurring discomfort, which helps them understand the urgency of surgery.
Gum Infections and Pain
Partially erupted teeth can trap bacteria beneath the gum line, leading to inflammation or pericoronitis. Persistent swelling or pain often prompts patients to look for information on early signs that extraction may be necessary. Removing the problematic tooth through an odontectomy can stop the cycle of infection and protect overall oral health.
Tooth Decay or Damage
If a tooth is badly decayed below the gum line or fractured, standard fillings or crowns may not suffice. Surgical removal ensures the problem does not worsen and prevents further complications.
Orthodontic Planning
In some cases, odontectomy is part of a broader dental plan to create space for proper alignment during orthodontic treatment.
The Odontectomy Procedure Step by Step
Understanding what happens during surgery can ease nerves and set realistic expectations.
Step 1: Consultation and Imaging
Before surgery, your oral surgeon evaluates your teeth and jaw using digital X-rays. These images show the position of the tooth, its relationship to surrounding bone, and whether nerves are nearby. This ensures a safe and precise procedure.
Step 2: Anesthesia and Comfort
Most patients receive local anesthesia, while some choose IV sedation for added comfort. Your surgeon will discuss options to ensure the procedure is as stress-free as possible.
Step 3: Accessing the Tooth
An incision is made in the gum to expose the tooth and any surrounding bone that may need to be removed. This step allows the surgeon to reach teeth that are fully or partially impacted.
Step 4: Tooth Removal
The tooth may be divided into smaller pieces for safer extraction. Each piece is carefully removed, minimizing trauma to surrounding tissue.
Step 5: Cleaning and Closure
The surgical site is cleaned, and stitches are placed to support healing. Most stitches dissolve on their own within one to two weeks.
Recovery and What to Expect
Recovery after an odontectomy varies, but most patients follow a predictable timeline.
First 24–48 Hours
Rest is crucial. Swelling, mild bleeding, and discomfort are normal. Ice packs and medications prescribed by your surgeon help manage pain and inflammation.
Days 3–5
Swelling usually peaks around day two or three and gradually improves. You may still experience tightness when opening your mouth, and soft foods are recommended.
One Week Post-Surgery
Most discomfort should diminish within seven days. Stitches begin to dissolve, and normal daily activities become easier.
Long-Term Healing
Although the gum surface heals quickly, underlying bone can take several months to fully recover. Maintaining oral hygiene and attending follow-up appointments ensures optimal healing.
Pain Management and Aftercare Tips
Follow Prescribed Medications
Take any pain relievers or antibiotics exactly as directed. Avoid aspirin immediately after surgery, as it can increase bleeding risk.
Gentle Oral Hygiene
Brush carefully around the surgical site and rinse with warm saltwater starting 24 hours after surgery. Proper cleaning helps prevent infection.
Soft Foods
Stick to soft foods like yogurt, mashed potatoes, oatmeal, and soups for the first few days. Avoid crunchy, hard, or spicy foods until fully healed.
Avoid Smoking and Straws
Using straws or smoking can dislodge the clot and increase the risk of dry socket, which is a painful complication.
Complex Cases and Special Considerations
Some odontectomy procedures require additional care:
Deeply Impacted Teeth
Teeth buried deep under the gum or bone may require more extensive surgery.
Nerve Proximity
Lower wisdom teeth are often near important nerves. Advanced imaging ensures the procedure avoids nerve damage.
Existing Infections
If infection is present, pre-surgery antibiotics may be prescribed to reduce swelling and promote safer healing.
Planning for the Future: Dental Implants and Costs
After tooth removal, many patients consider long-term solutions like dental implants. Understanding costs and insurance coverage helps plan effectively.
Insurance Considerations
Patients often check implant insurance guides to see whether implants are covered, which helps reduce surprise expenses.
Cost Planning
Reviewing a cost guide for tooth extractions or implants allows patients to budget for treatment effectively.
Finding a Specialist
For those considering replacements, researching implants near their location ensures they connect with qualified professionals.
When to Call Your Oral Surgeon
Contact your surgeon if you notice:
- Persistent or heavy bleeding
- Severe pain beyond a few days
- Pus or unusual discharge
- Fever or chills
- Trouble swallowing or breathing
Early intervention ensures minor complications do not become serious.
Schedule a Call
Our Office
3860 Southwest 8th Street Ste. 201 Coral Gables, FL, 33134 United States
Business Hours
Monday thru Friday 9am-5pm
Office #
305-552-1193
FAX #
305-328-9630
Email #
drcaceres@oralfacialsurgery.miami
Final Thoughts
An odontectomy is a routine but important procedure that protects your long-term oral health. Whether you’re dealing with impacted wisdom teeth, recurring infections, or early signs, understanding the process and recovery helps you feel prepared and confident.
Considering future dental needs, including implants, costs, and insurance, is a smart step toward maintaining your smile after surgery. By following aftercare instructions and attending follow-ups, most patients recover smoothly and enjoy lasting oral health.

Do Wisdom Teeth Cause Crooked Teeth?
January 5, 2026

Wisdom Tooth Pain vs. a Regular Toothache: How to Tell the Difference
November 17, 2025

How Rare Are Serious Wisdom Tooth Complications, Really?
December 18, 2025
Signs Your Wisdom Tooth Is Growing the Wrong Way
February 9, 2026
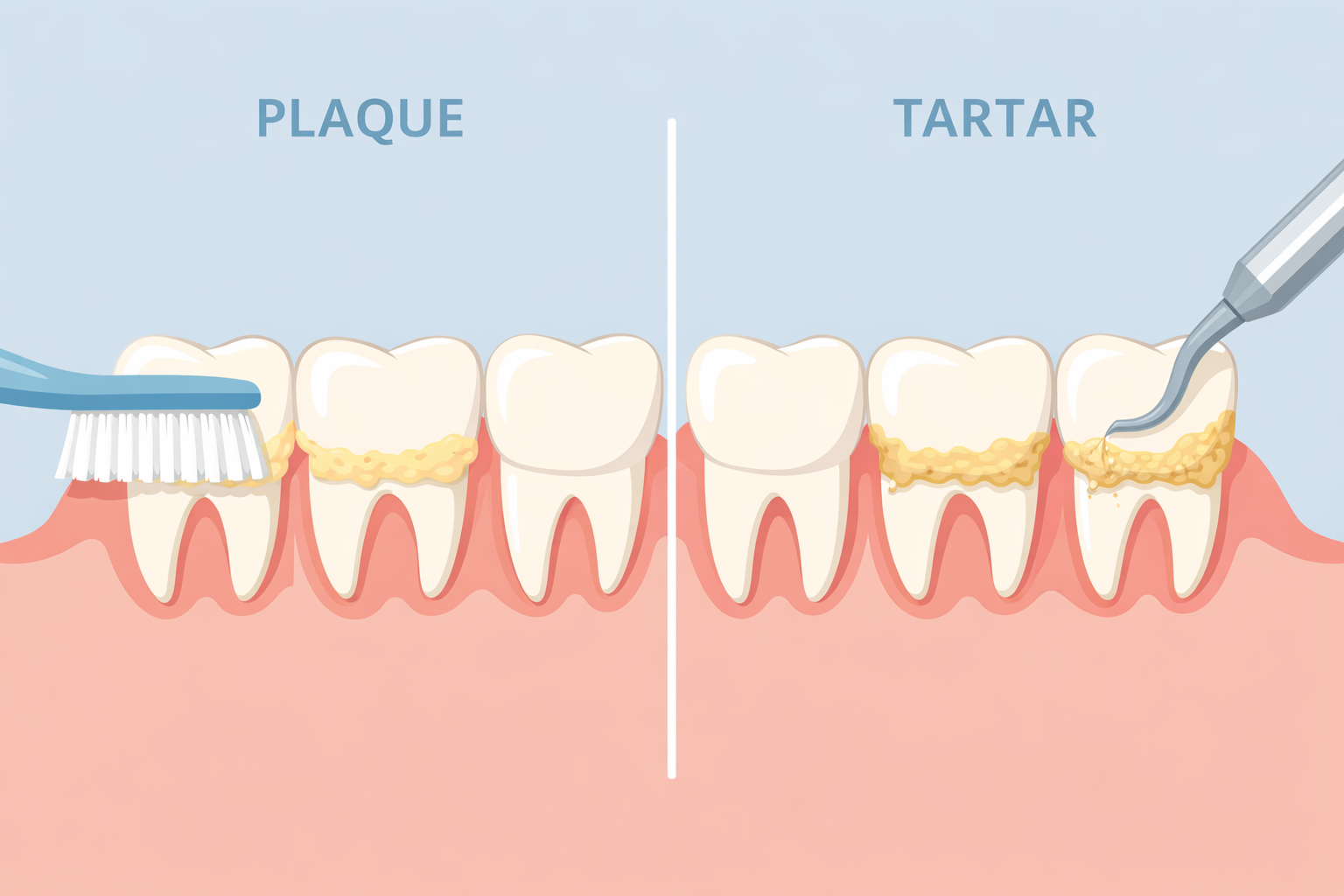
Plaque vs. Tartar: What’s the Difference?
January 16, 2026