How to Tell If Your Wisdom Tooth Is Infected

Wisdom teeth can be tricky. While some people experience no issues, others may face pain, swelling, or infections that affect their daily life. Recognizing the signs of a wisdom tooth infection early can prevent complications and help you seek timely treatment. In this guide, we’ll explore how to tell if your wisdom tooth is infected, what causes infections, and the best ways to manage them.
Understanding Wisdom Teeth and Their Role
Wisdom teeth, also called third molars, typically appear between the ages of 17 and 25. These teeth often emerge at awkward angles due to limited space in the jaw, which can lead to crowding, impaction, or partial eruption. When wisdom teeth do not fully break through the gums or grow in misaligned, they create pockets where bacteria can thrive, increasing the risk of infection. To learn more about teeth growing at the wrong angle, see our guide on wisdom tooth growth.
Why Wisdom Teeth Are Prone to Infection
Impacted or partially erupted wisdom teeth are particularly vulnerable because food particles and bacteria can get trapped around them. This environment encourages bacterial growth, which can lead to pericoronitis, gum inflammation, or abscess formation. Without proper care, the infection can spread, causing more severe dental and systemic issues.
Common Signs Your Wisdom Tooth May Be Infected
Recognizing the symptoms of an infected wisdom tooth early is crucial for preventing complications. Some of the most common signs include:
Persistent Pain or Discomfort
A dull, throbbing, or sharp pain at the back of your mouth is often the first sign of infection. Pain may radiate to your jaw, ear, or neck. Discomfort that worsens when chewing or opening your mouth widely should never be ignored. In cases where extraction is necessary, understanding simple vs surgical options can help you prepare.
Swelling and Redness
Infections often trigger swelling around the affected tooth or surrounding gums. You may notice redness, tenderness, or puffiness in the back of your mouth. Swelling can sometimes extend to your face or jaw, indicating a more severe infection.
Gum Tenderness or Bleeding
Gums around an infected wisdom tooth may become sensitive or bleed easily, especially when brushing or flossing. This inflammation is a sign that your immune system is responding to bacterial activity in the area.
Bad Breath or Unpleasant Taste
Infections often produce pus or bacterial buildup, which can lead to chronic bad breath or a metallic, foul taste in the mouth. If brushing and rinsing do not alleviate these symptoms, it may indicate a deeper issue.
Difficulty Opening Your Mouth or Swallowing
Severe infections can cause trismus, a condition where jaw movement becomes limited and painful. You may also experience difficulty swallowing or a feeling of fullness in your jaw.
Fever or Swollen Lymph Nodes
A spreading infection can trigger a mild to moderate fever and swollen lymph nodes in the neck. This indicates that your body is fighting off bacteria and that prompt professional care is needed.
Risk Factors That Increase the Likelihood of Infection
Certain conditions make wisdom tooth infections more likely. Being aware of these risk factors can help you take preventive measures:
- Impacted Teeth: Teeth that grow at an angle and fail to fully emerge are more prone to bacterial accumulation.
- Poor Oral Hygiene: Neglecting to brush and floss properly can increase the risk of infections.
- Weakened Immune System: Conditions such as diabetes or autoimmune disorders can make it harder for your body to fight infections.
- History of Gum Disease: Previous periodontal issues can predispose you to complications around wisdom teeth.
How to Prevent Wisdom Tooth Infections
Prevention is always better than cure. Here are some ways to reduce the risk of infection:
Maintain Proper Oral Hygiene
Brush at least twice a day and floss daily, paying extra attention to the back of your mouth where wisdom teeth reside. Consider using an antiseptic mouthwash to reduce bacterial buildup.
Schedule Regular Dental Check-Ups
Routine dental visits allow your dentist to monitor wisdom teeth growth, identify potential problems, and intervene before infections occur. X-rays can help detect impacted teeth that may cause trouble. You may also read about why removal isn’t always needed for certain cases.
Use Saltwater Rinses
Rinsing your mouth with warm saltwater can soothe irritated gums, reduce swelling, and kill some bacteria in the oral cavity. This can be especially helpful if a tooth is partially erupted.
Avoid Smoking and Tobacco
Smoking compromises your oral health and slows healing, making infections more likely. Eliminating tobacco products can reduce the risk significantly.
Treatment Options for an Infected Wisdom Tooth
If you suspect an infection, timely professional care is essential. Common treatments include:
Antibiotics
A dentist may prescribe antibiotics to reduce bacterial infection and inflammation. This is often a short-term solution to manage pain and prevent the spread of infection before further procedures.
Drainage of Abscesses
If a pus-filled abscess forms, your dentist may need to drain it to relieve pressure and remove bacteria. This can significantly reduce pain and swelling.
Wisdom Tooth Extraction
In many cases, removing the problematic wisdom tooth is the most effective long-term solution. Extractions prevent recurring infections and alleviate pressure on surrounding teeth. Check our tips on recovery after removal to support healing. Be aware of complications like dry socket and how to prevent them.
Pain Management
Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help manage discomfort while awaiting treatment. Always follow dosage guidelines and consult your dentist if symptoms persist.
When to Seek Immediate Dental Care
Some infections can escalate rapidly, so it’s important to seek urgent professional help if you experience any of the following:
- Severe facial swelling
- Difficulty breathing or swallowing
- High fever
- Spreading infection to other areas of the head or neck
If you notice these symptoms, contact our office promptly for evaluation and treatment. You can reach us at:
Our Office:
3860 Southwest 8th Street Ste. 201, Coral Gables, FL, 33134, United States
Business Hours:
Monday thru Friday, 9am–5pm
Office #: 305-552-1193
FAX #: 305-328-9630
Email #: drcaceres@oralfacialsurgery.miami
Prompt intervention can prevent serious complications and ensure a smoother recovery.
Recovery and Aftercare
After treatment, follow these steps to support healing:
- Take prescribed medications as directed
- Keep the area clean with gentle rinsing
- Avoid hard or sticky foods that can irritate the site
- Rest and maintain hydration to support your immune system
- Attend follow-up appointments to monitor recovery
Final Thoughts
Wisdom tooth infections are painful but manageable with timely recognition and proper care. By understanding the signs, practicing preventive measures, and seeking prompt professional treatment, you can protect your oral health and reduce the risk of complications. Don’t ignore persistent pain or swelling in the back of your mouth—early action is key.

How Much Does Wisdom Teeth Removal Really Cost?
November 19, 2025

Wisdom Tooth Removal and Sinus Issues: What’s Really Going On?
December 25, 2025
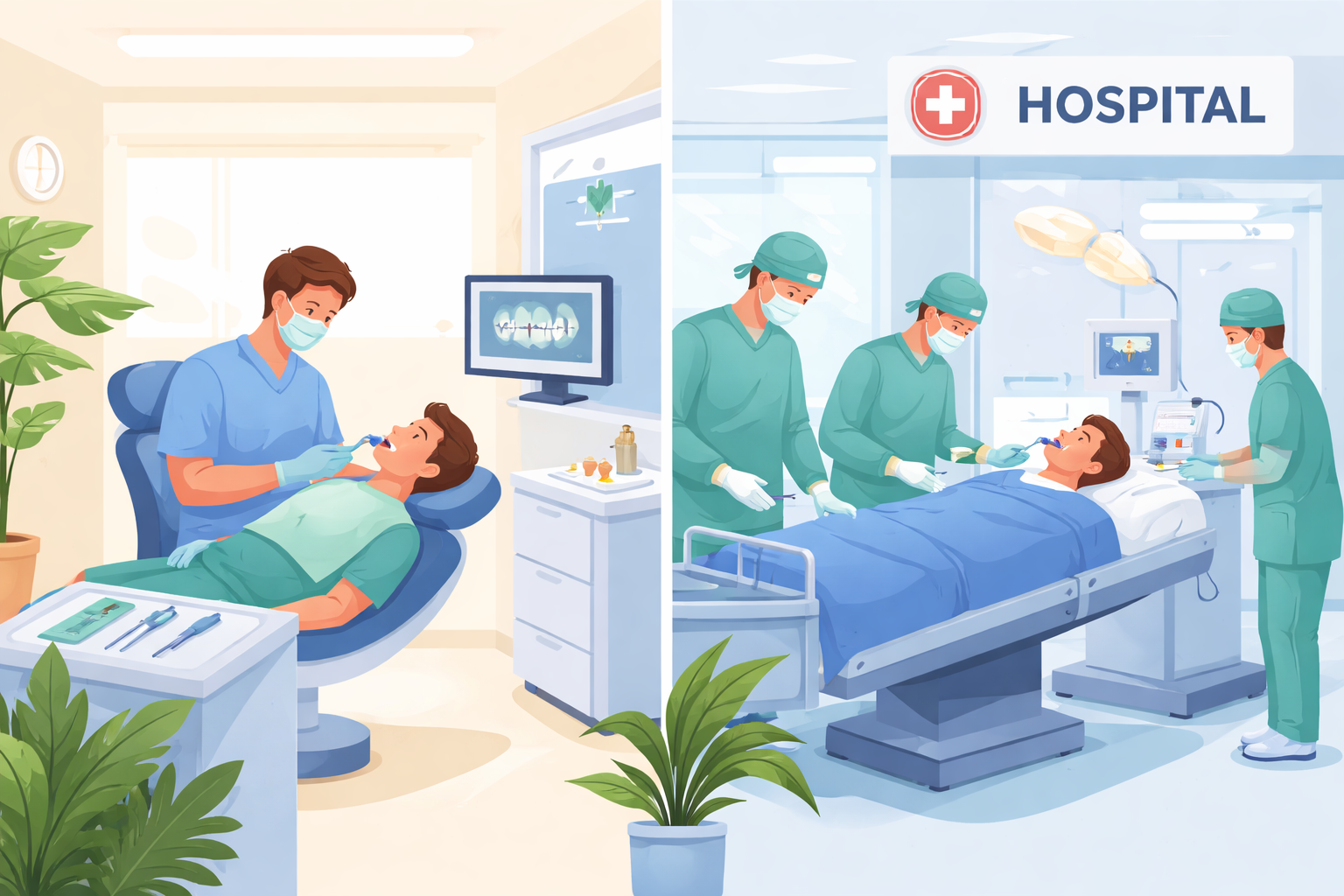
Comparing In-Office vs. Hospital Wisdom Tooth Extraction Costs
January 28, 2026

Facial Swelling and Tooth Pain: How to Know When It’s an Emergency
January 8, 2026

Post-Surgery Red Flags Parents Should Watch For
December 22, 2025