When a Tooth Can’t Be Saved?

Losing a natural tooth is never the outcome anyone hopes for. Modern dentistry focuses heavily on saving teeth whenever possible, using treatments like fillings, crowns, and root canals to preserve structure and function. Still, there are situations where damage, infection, or bone loss reaches a point where a tooth simply cannot be saved. When that happens, removing the tooth is often the safest and healthiest decision for your long-term oral health.
Understanding when a tooth cannot be saved, why extraction may be necessary, and what options exist afterward can ease anxiety and help you make confident, informed decisions. This article walks through the most common reasons teeth become non-restorable, how oral surgeons evaluate these cases, and what life looks like after removal.
Why Saving a Tooth Isn’t Always Possible
Dentists and oral surgeons prioritize conservative care. The goal is always to maintain as much of your natural tooth structure as possible. However, certain conditions make restoration unreliable or unsafe.
Severe Tooth Decay Beyond Repair
Tooth decay becomes a serious problem when it penetrates deep into the structure of the tooth. If decay reaches below the gum line or destroys most of the remaining enamel and dentin, there may not be enough healthy structure left to support a crown or filling.
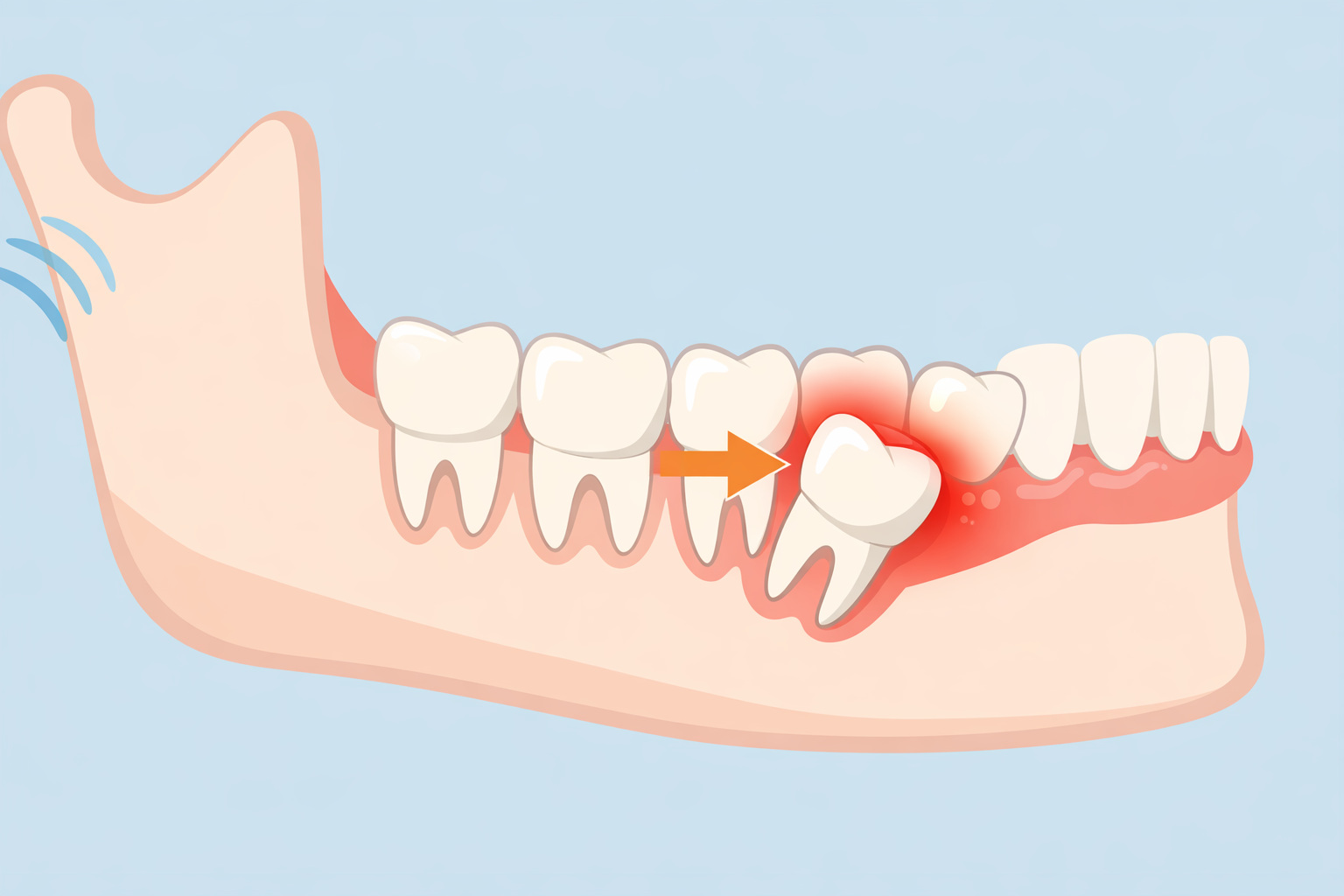
In advanced cases, bacteria can spread rapidly, compromising nearby bone and teeth. Attempting to save a tooth in this condition often leads to recurring infections and repeated dental work. Patients experiencing persistent pain can learn more about wisdom tooth infection to understand how untreated dental infections develop.
Deep Infections and Abscesses
Infections that originate inside the tooth or at the root tip can sometimes be treated with root canal therapy. However, when an infection spreads extensively into surrounding bone or soft tissue, the tooth may become a constant source of inflammation.
Signs of serious infection often include swelling, persistent pain, drainage, and fever. Early identification is crucial; noticing early signs can help prevent serious complications.
Cracked or Fractured Teeth Below the Gum Line
Cracks that extend beneath the gum line or into the root are particularly problematic. Unlike surface cracks, these fractures allow bacteria to enter areas that cannot be sealed or cleaned properly.
Vertical root fractures almost always require extraction. Even if pain comes and goes, the damage compromises the tooth’s integrity permanently.
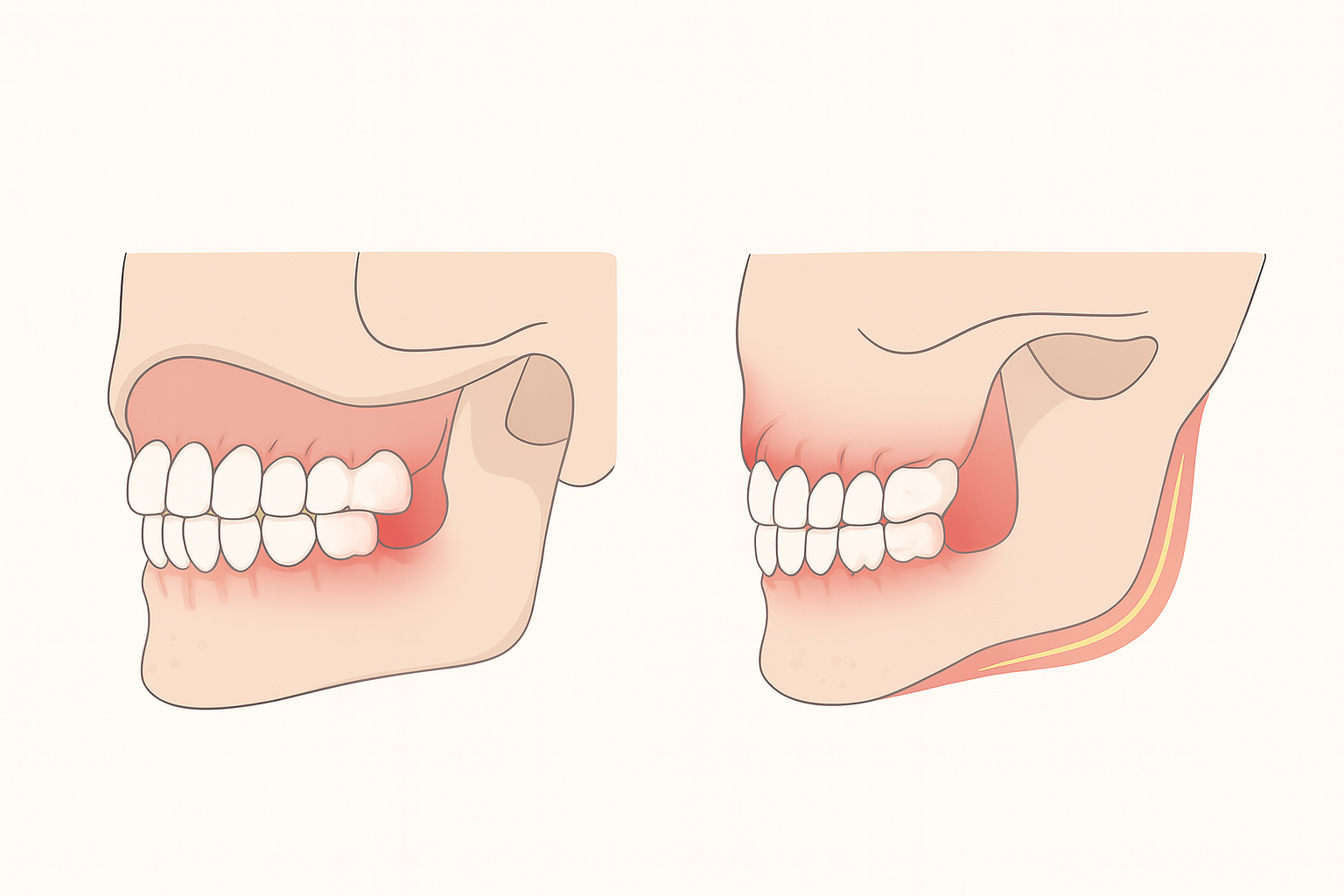
Advanced Gum Disease and Bone Loss
Periodontal disease weakens the foundation that holds teeth in place. When bone loss becomes severe, teeth may loosen and shift. Even if the tooth itself is structurally sound, it cannot function without adequate bone support.
At this stage, removing the tooth may help preserve surrounding bone and prevent infection from spreading to neighboring teeth.
How Dentists Decide a Tooth Cannot Be Saved
Comprehensive Examination and Imaging
Before recommending extraction, dentists and oral surgeons rely on detailed exams and diagnostic imaging. Digital X-rays and 3D scans reveal damage below the surface, including bone loss, root fractures, or infection spread.
This careful evaluation ensures extraction is recommended only when restoration would be unpredictable or harmful.
Assessing Long-Term Prognosis
A key factor is whether a treated tooth will remain stable over time. If a tooth requires extensive work but still carries a high risk of failure within a few years, extraction may be the more reliable option.
Insurance coverage can influence decision-making. Learning how dental implants are covered helps patients plan financially for replacements after extraction.
Common Situations Where Extraction Is the Best Choice
Repeated Treatment Failures
If a tooth has undergone multiple procedures, such as root canals or crown replacements, yet continues to cause pain or infection, it may no longer be viable. Repeated interventions often weaken remaining tooth structure.
Impacted or Problematic Wisdom Teeth
Wisdom teeth are frequently removed because of positioning, infection risk, or damage to neighboring teeth. When decay or infection becomes severe, saving them is rarely practical. Understanding removal costs can also help patients prepare financially.
Trauma or Injury
Accidents can cause teeth to shatter or dislodge. If the root or surrounding bone is severely damaged, stabilizing the tooth may not be possible.
What Happens During a Tooth Extraction
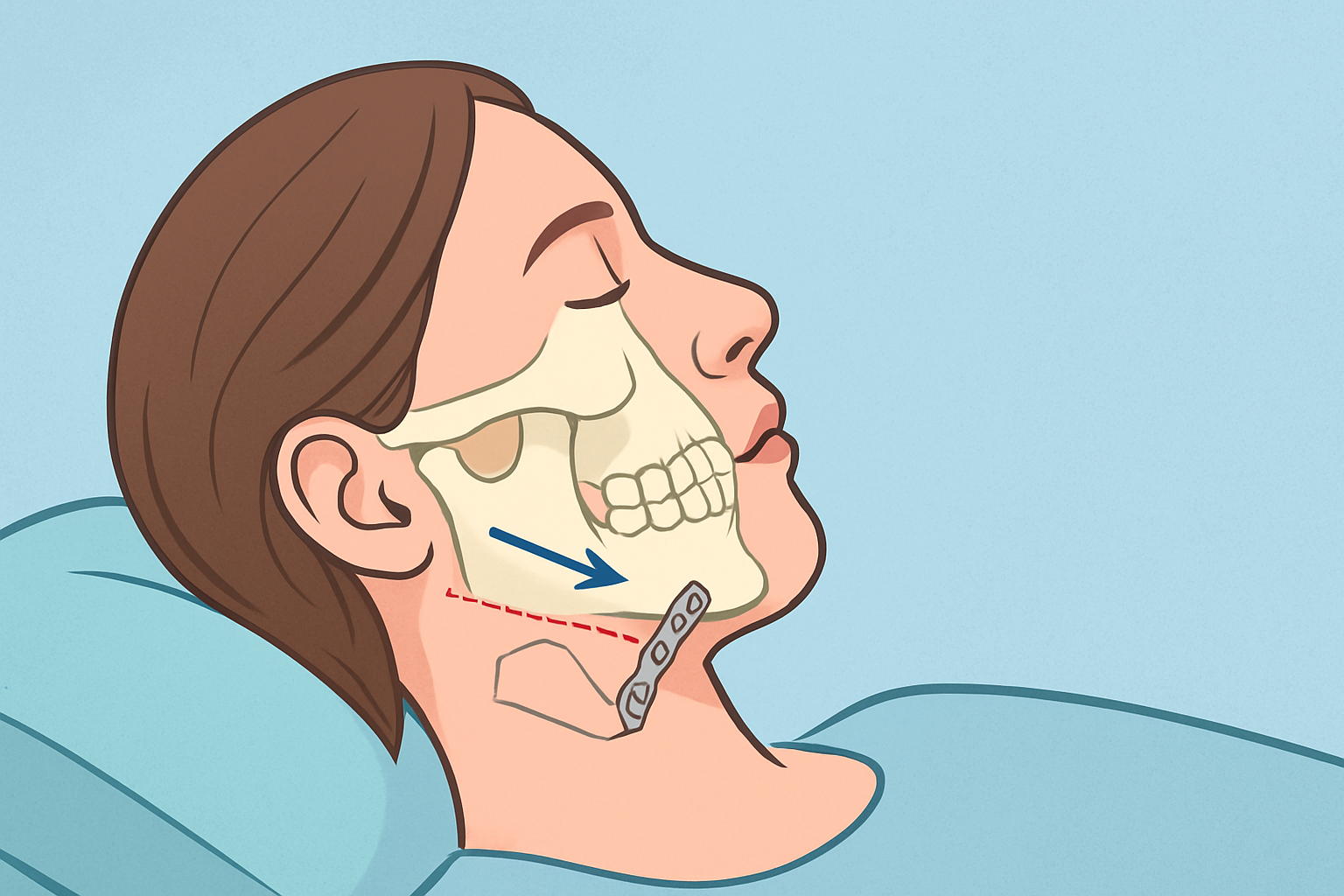
Simple vs Surgical Extractions
Some teeth can be removed with a straightforward procedure under local anesthesia. Others, especially broken or impacted teeth, require surgical extraction performed by an oral surgeon.
Surgical extractions involve small incisions and, in some cases, sectioning the tooth to remove it safely.
Comfort and Sedation Options
Most patients are surprised by how comfortable modern extraction procedures are. Sedation options range from local anesthesia to IV sedation, ensuring pain and anxiety are well controlled.
Recovery After a Tooth Cannot Be Saved
The First 24 to 72 Hours
Initial healing focuses on clot formation and inflammation control. Mild swelling, soreness, and limited bleeding are normal.
Following post-operative instructions closely helps reduce complications and speeds healing.
Avoiding Complications
Dry socket, infection, and delayed healing are potential risks. Avoid smoking, using straws, or vigorous rinsing during the early healing phase.
Good oral hygiene and proper nutrition support recovery.
Replacement Options After Tooth Loss
Losing a tooth does not mean living with a gap permanently. Several reliable solutions restore function and appearance.
Dental Implants
Dental implants are considered the gold standard for replacing missing teeth. They integrate with the jawbone, providing stability similar to a natural tooth.
Bridges and Partial Dentures
For some patients, bridges or removable partial dentures provide effective alternatives. These options may be appropriate depending on bone health, budget, and overall oral condition.
Emotional Impact of Losing a Tooth
Addressing Anxiety and Uncertainty
Being told a tooth cannot be saved can feel overwhelming. It is normal to worry about appearance, pain, or long-term effects.
Clear communication with your dental provider helps ease concerns and ensures you understand each step of the process.
Focusing on Long-Term Health
While saving a tooth is ideal, removing a compromised tooth often prevents more serious problems later. Eliminating chronic infection protects overall health and improves comfort.
When to Seek an Oral Surgeon’s Opinion
Some cases require specialized care, particularly when infection, bone loss, or impacted teeth are involved. Oral surgeons have advanced training in complex extractions and reconstruction.
Seeking expert evaluation early can prevent complications and preserve future treatment options.
Moving Forward After Tooth Removal
When a tooth cannot be saved, extraction is not a failure of care. It is often a proactive step toward restoring balance, comfort, and oral health.
With today’s advanced replacement options, patients can return to eating, speaking, and smiling with confidence. The key is timely intervention, thoughtful planning, and working with experienced dental professionals who prioritize long-term results.
Do Upper and Lower Wisdom Teeth Hurt Differently?
December 11, 2025

Early vs. Late Wisdom Tooth Removal: Which Is Better?
January 7, 2026

Is Wisdom Tooth Removal Painful? Real Patient Guide
February 13, 2026
Jaw Surgery Risks and Benefits: What You Should Know Before Going Under
November 24, 2025
What Really Happens If You Don’t Remove Problem Wisdom Teeth
January 16, 2026