Wisdom Tooth Pain vs. a Regular Toothache: How to Tell the Difference

When a sudden pain hits your mouth, it can be tough to know what you’re dealing with. Is it normal tooth sensitivity? A cavity? Or is your wisdom tooth finally trying to break through? Because the mouth has many nerves packed into a small space, different types of dental pain can feel similar, making it easy to misinterpret the symptoms.
This guide breaks down the key differences between wisdom tooth pain and a regular toothache so you can understand what’s happening, when to take action, and how to get relief. Whether you’re dealing with swelling, pressure, gum soreness, or sharp throbbing pain, this article will clarify what your symptoms really mean and the next steps you should take.
Why It’s Important to Know the Difference
Not all dental pain is treated the same way. Wisdom tooth pain often requires oral-surgery-level evaluation, while common toothaches could point to cavities, gum infections, or nerve irritation. Acting early can prevent complications such as:
- Gum infections around the wisdom tooth
- Cysts or damage to nearby teeth
- Severe tooth decay
- Abscess formation
- Prolonged inflammation and jaw discomfort
Knowing the source of your pain helps you avoid unnecessary suffering and ensures you get the right treatment before the problem escalates.
Understanding Wisdom Teeth and Why They Hurt
Wisdom teeth are the last set of molars to emerge, usually appearing between ages 17 and 25. While some people never feel a thing, many experience discomfort because these teeth often don’t have enough room to grow properly.
Common Causes of Wisdom Tooth Pain
1. Eruption Pain
As the tooth pushes through the gums, it creates soreness and pressure in the back of the jaw.
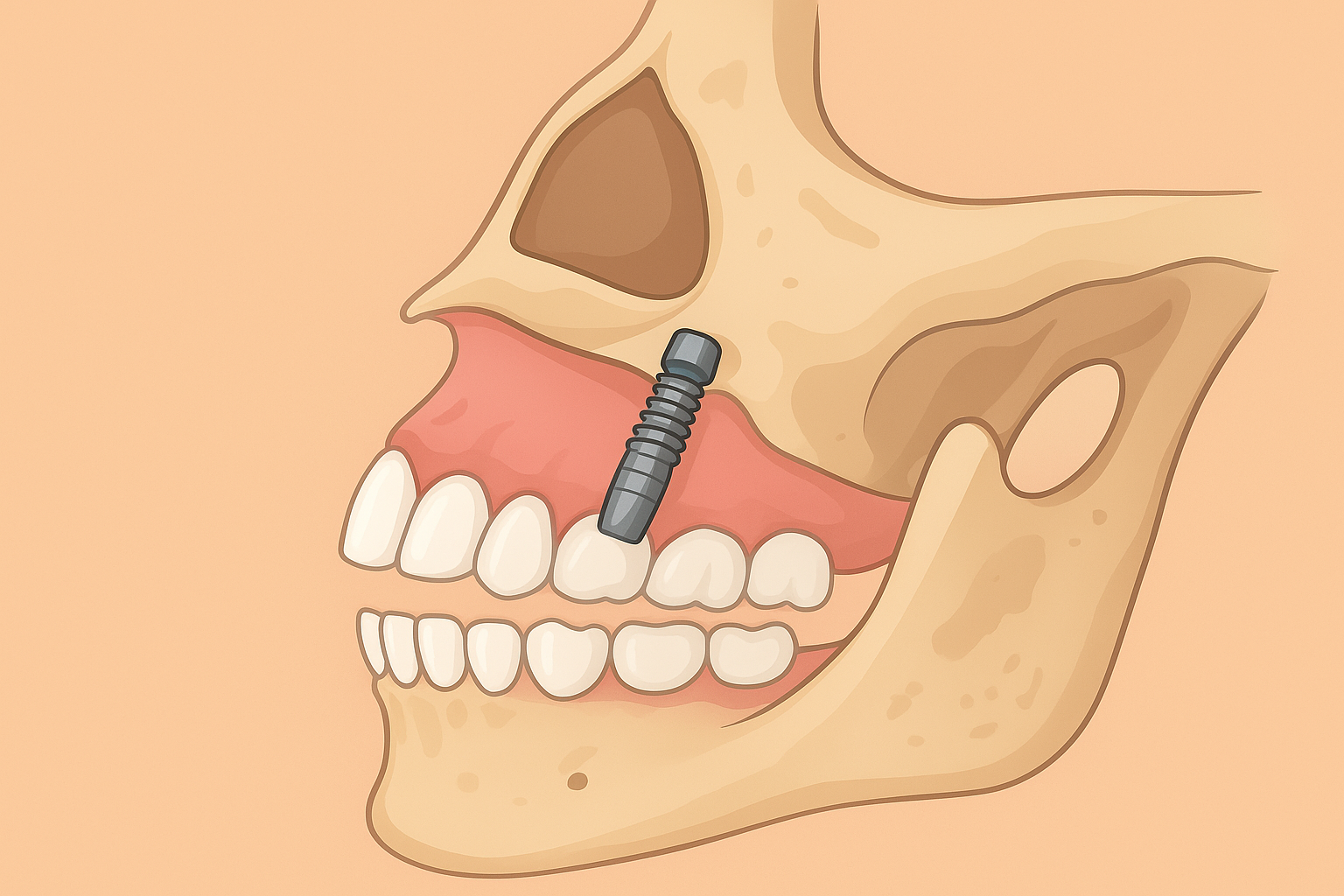
2. Impacted Wisdom Teeth
If the tooth grows sideways or stays stuck under the gum, it can cause sharp, persistent pain. For a deeper look into how to tell if your wisdom tooth is growing wrong, check out our post on how to know if your wisdom tooth is growing wrong.
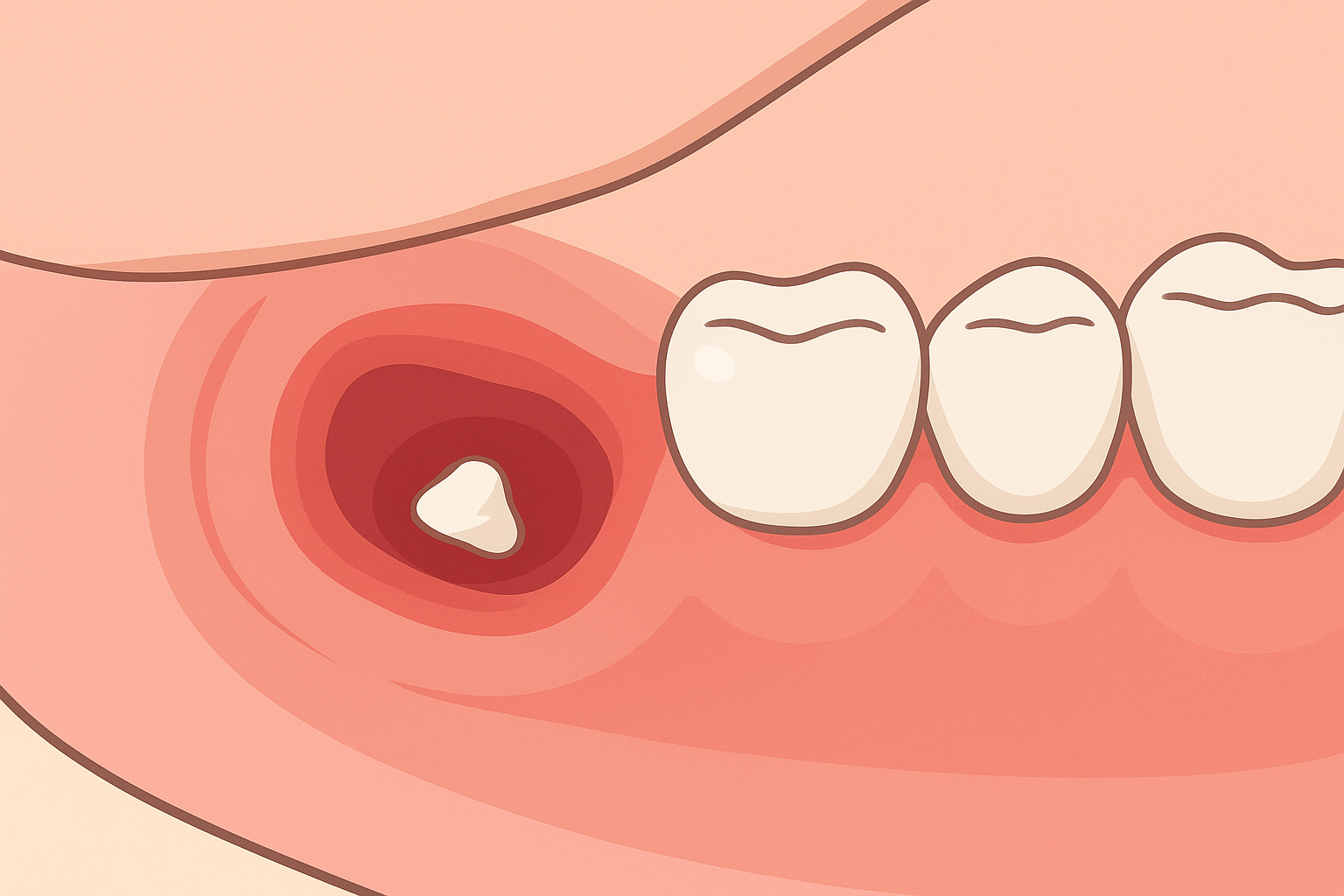
3. Pericoronitis
This is a common gum infection triggered by partially erupted wisdom teeth. Food and bacteria get trapped under the gum flap, causing swelling, redness, and a bad taste in the mouth. For after-removal swelling and healing complications, you may also want to read more about swelling after wisdom tooth removal in Florida heat.
4. Pressure on Nearby Teeth
Wisdom teeth can push against the molars next to them, causing jaw discomfort and crowding.
5. Cysts or Tissue Inflammation
In rare cases, cysts can form around impacted wisdom teeth, leading to more serious pressure and pain.
These causes tend to create pain that is deeper, harder to ignore, and often accompanied by swelling at the very back of your mouth.
What a Regular Toothache Usually Means
A typical toothache is often related to the structure of the tooth itself—not new teeth erupting. Pain can come from:
- Cavities
- Cracked or chipped teeth
- Exposed dentin
- Sensitivity to hot or cold
- Gum disease
- Tooth abscess
- Worn-down enamel
- Grinding or clenching
Most of these issues cause localized discomfort around one tooth, and the pain typically worsens during chewing, exposure to temperature changes, or at night when blood flow increases to the head.
Wisdom Tooth Pain vs. Regular Toothache: The Key Differences
Although both types of pain can be intense, there are clear symptoms that help you tell them apart.
1. Location of the Pain
Wisdom Tooth Pain
- Located at the very back of the mouth
- Often affects the jaw, ear, or neck
- Sometimes radiates to the side of the face
Regular Toothache
- Coming from a specific tooth (front or back)
- Rarely spreads to the ear or neck
- Pain feels more focused and identifiable
If the pain feels like it’s behind your last molar or deep in your jaw, it’s probably wisdom-tooth related.
2. Type of Pain
Wisdom Tooth Pain
- Throbbing pressure
- Sharp stabbing pain when biting
- Soreness in the jaw
- A feeling of “something pushing” at the back teeth
- Discomfort that worsens when chewing in the back
Regular Toothache
- Sharp pain triggered by hot or cold foods
- Sudden shooting shocks
- Constant pulsing in one tooth
- Sensitivity to sweets
- Painful chewing in one specific area
3. Gum Condition
Wisdom Tooth Pain
- Swollen gums behind the molars
- Redness or gum flaps (pericoronitis)
- Bad taste or odor
- Possible difficulty opening the mouth fully
Regular Toothache
- Gum swelling near the affected tooth
- Bleeding during brushing (gum disease)
- No gum flap present
- Sensitivity near the gumline
4. Swelling and Facial Pressure
Wisdom Tooth Pain
Swelling is more common because of inflammation around erupting or impacted teeth. This swelling may be felt:
- In the jaw
- Near the ear
- Under the jawline
Regular Toothache
Swelling generally happens only with more severe infections or abscesses but is usually localized near the specific tooth.
5. Difficulty Opening the Mouth (Trismus)
This symptom is strongly associated with wisdom teeth, especially impacted ones. A regular toothache rarely causes jaw stiffening unless an advanced infection is present.
6. Taste and Smell Issues
Wisdom Tooth Pain
If the gum around a wisdom tooth becomes infected, you may notice:
- Bad breath
- A foul taste
- Pus or discharge
Regular Toothache
Bad taste occurs primarily when an abscess is present.
When Wisdom Tooth Pain Needs Urgent Attention
While wisdom tooth discomfort is common, certain symptoms mean you should contact a dentist or oral surgeon immediately:
- Severe swelling around the jaw
- Difficulty swallowing
- Fever or chills
- Pus or discharge
- Persistent throbbing pain
- Difficulty opening your mouth
- Pain that interferes with eating or sleeping
Because wisdom teeth sit so close to nerves and jaw structures, delaying care can lead to serious complications.
You may also want to read more about recovery tips after wisdom teeth removal, especially if you think extraction might be in your future.
When a Regular Toothache Needs Immediate Care
A standard toothache also becomes an emergency when:
- The pain is severe or unrelenting
- There’s visible decay or a cracked tooth
- You experience sudden sensitivity to pressure
- Swelling spreads around the cheek
- You see a pimple-like bump on the gum (abscess)
Ignoring decay or infection can lead to nerve damage or tooth loss.
How Dentists Diagnose the Difference
To confirm the cause of your pain, your dentist will typically:
1. Ask About Your Symptoms
They’ll assess location, severity, and triggers.
2. Examine the Back of Your Mouth
Checking for swollen gums, inflammation, partial eruption, or infection.
3. Take X-Rays
Panoramic or 3D imaging can reveal:
- Impacted wisdom teeth
- Cysts
- Cavities
- Deep decay
- Abscesses
- Bone loss
X-rays are the most reliable way to distinguish between the two issues.
If extraction is needed, your oral surgeon will evaluate whether this is a simple vs. surgical extraction — learn more about the differences between simple and surgical extractions.
They’ll also decide what kind of anesthesia is best for you. For example, our guide on types of anesthesia for wisdom tooth removal goes into how local, IV, or general sedation may be used.
Treatment Options for Wisdom Tooth Pain
Treatment depends on the cause. Common solutions include:
- Warm Saltwater Rinse — Helps soothe irritated gums.
- Pain Relievers — Over-the-counter anti-inflammatory medicine helps reduce pain and swelling.
- Antibiotics — Used if there’s infection, but often just a bridge until extraction.
- Cleaning the Gum Flap — Dentists can remove trapped debris causing pericoronitis.
- Extraction — Many wisdom tooth pain issues don’t resolve until removal, especially for impacted or repeatedly infected teeth.
After removal, how well you heal depends a lot on your habits. For example, smoking can delay recovery. You might be interested in reading about how smoking affects wisdom tooth healing.
Treatment Options for a Regular Toothache
Typical treatments vary based on what’s causing the pain:
- Fillings for cavities or minor decay
- Root Canal Treatment if the nerve is infected or inflamed
- Crowns for cracked or heavily worn-down teeth
- Scaling/Deep Cleaning when gum disease is behind the pain
- Extraction only if the tooth is beyond repair
Home Remedies for Short-Term Relief
While these don’t replace a dentist’s care, they can help ease symptoms temporarily:
For Wisdom Tooth Pain:
- Ice packs applied to the jaw
- Warm saltwater rinses
- Keeping the area clean behind the last molar
- Avoiding very hard or chewy foods
- Using an antiseptic or gentle mouthwash
For Regular Toothache:
- Over-the-counter pain relievers
- Clove oil (gently applied)
- Avoiding extreme hot or cold foods
- Keeping the tooth area free of food debris
If pain continues beyond a day or two, it’s time to get a dental evaluation.
Can Wisdom Tooth Pain Feel Like a Normal Toothache?
Absolutely. In some cases, wisdom tooth pain can be misinterpreted as a simple cavity or sensitivity — especially when the discomfort radiates to nearby teeth. What often gives it away is:
- Deep pain located behind the last molar
- Gum inflammation or redness in that area
- Discomfort increases when chewing in the back
If your symptoms match, it’s more likely that your wisdom teeth (perhaps impacted) are the real cause, rather than a standard tooth issue.
How to Prevent Future Pain
Prevention helps a lot — here are some steps to keep both wisdom tooth pain and common toothaches at bay:
To Prevent Wisdom Tooth Pain:
- Schedule regular dental checkups
- Request X-rays every 1–2 years to monitor wisdom tooth growth
- Treat early signs of infection like pericoronitis
- Discuss preventive removal if teeth are impacted
To Prevent Regular Toothaches:
- Maintain consistent brushing and flossing
- Visit the dentist twice a year
- Treat sensitivity early (don’t ignore it)
- Avoid habits that damage enamel (grinding, crunching on hard foods)
- Address cavities or gum disease before they escalate
Final Thoughts
Tooth pain can be confusing, but knowing whether it’s wisdom tooth pain or a regular toothache helps you take the right steps. Wisdom tooth discomfort often shows up as pressure deep in the jaw, swelling, and possible gum inflammation — while typical toothaches tend to feel more localized, especially around one tooth.
If you’re ever unsure, it’s best to talk to your dentist. They’ll help you figure out what’s really going on, and guide you on next steps — whether that’s monitoring, treatment, or extraction. Early diagnosis and timely care make a big difference in how quickly you can get back to pain-free living.
You may also want to read more about common myths about wisdom tooth removal and how they might influence your decision: check out our article on common myths about wisdom tooth removal.
Can Wisdom Teeth Grow Back After Removal?
December 9, 2025

What Is an Odontectomy? A Clear Guide to Wisdom Tooth Surgery
February 26, 2026
Zygomatic Implants: Your Guide to a Stronger Implant Solution
November 26, 2025

Cheap vs Quality Wisdom Tooth Removal: What Really Matters?
December 18, 2025

Oral Pathology: When a Biopsy Is Required and What to Expect
January 21, 2026